Francesca Lyon, Director of Nutrition at FUTURE WOMAN explores a surprising reason you may be feeling run down every winter. And it might not be your immune system that’s the problem, it could be your hormones. Francesca explores how cortisol, estrogen, progesterone (and even testosterone!) shape your immune strength, and what you can do to support them naturally.
What if there was a way to bolster your immune system and support you through the winter months? And no it doesn’t involve taking the latest trendy supplement or ice plunging (no thanks!)… but simply involves supporting your hormones?
Your immune system is often oversimplified and thought of as a simple defense army – fighting off germs, infections, and illnesses. But the reality is far more complex. One of the most powerful influences on your immune health isn’t just what you eat or how much you sleep but it’s your hormones!
These hormones and chemical messengers orchestrate nearly every function in your body, from how you feel, sleep, your appetite and even how well you build muscle. But they also impact how your immune system responds to threats.
You may have already heard of cortisol (your stress hormone) and its connection to inflammation and the immune system, but estrogen, progesterone and other hormones like testosterone have a huge impact too.
Understanding how hormones impact immunity isn’t just really interesting ( I may be biased here..!) but it is also practical. By optimising our hormone production and levels we can support immune resilience as we move into the colder months. In this article, we’ll explore the key hormones that influence your immune system so we can support your body’s defences naturally.
Cortisol and Stress
We have all experienced how when we are stressed we seem to get sick more…. So let’s start with our stress hormone cortisol. Cortisol is often referred to as our stress hormone as it is released from the adrenal glands in response to a perceived stress or threat, this includes a threat from immune activity.
Cortisol when activated short term is incredibly beneficial for our immune system as it:
- Suppresses pro-inflammatory cytokines: Cortisol inhibits the release of pro-inflammatory cytokines, such as IL-6 and TNF-α.
- Promotes anti-inflammatory cytokines: It also promotes the production of anti-inflammatory cytokines like IL-10, which help to reduce inflammation.
- Regulates and recruits immune cells: Cortisol can influence and recruit various immune cells by reducing their activity or promoting them to achieve a more balanced immune response in turn regulating the immune system.
So what happens when cortisol is too high or low?
| Essentially if cortisol is too high (acute stress) or too low (long-term chronic stress) it can lead to suppression of the adaptive immune system (reduction in activity of T-cells and B-cells, reduced antibody activity and overall reduction in ability to fight illness and infections. It also results in overall immune dysregulation meaning the body is more susceptible to infections and illness and even autoimmune disease. |
If cortisol is activated and released longer term (whether from real or perceived stress or continuous activation of the immune system) this can lead to high levels of cortisol which leads to the inhibition of pro-inflammatory cytokines which means the body doesn’t get the healthy inflammatory response it needs to regulate the immune system.

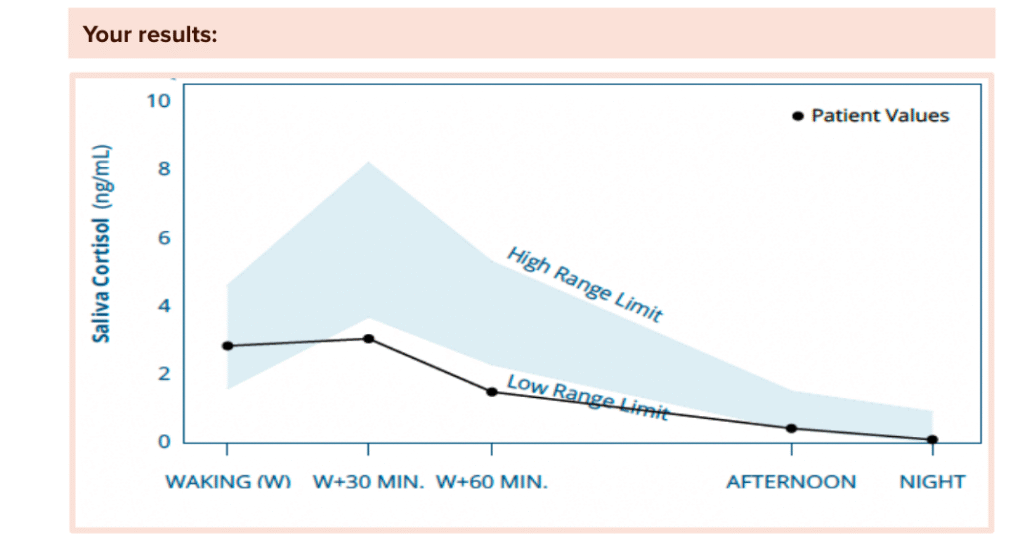
As we have seen with many FUTURE WOMAN clients – long term stress can also lead to a low cortisol levels which results in symptoms such as insomnia, mood changes, missing periods, worsening perimenopausal and menopausal symptoms and of course immune system issues like recurring infections too. When cortisol is low it cannot respond properly to the immune threats, therefore the body is more susceptible to infections, impaired wound healing, and chronic inflammatory conditions (including things like PCOS and worsening perimenopausal symptoms!).
Example of a client’s test results with lower cortisol. This client suffered from recurrent UTI’s, eczema and colds.
Estrogen’s helpful immune ‘boost’:
Now let’s look at estrogen. It is not often people think of estrogen as helpful to our immune system, but it has a very important role to play in enhancing immune response. First it is important to know that we have estrogen receptors in nearly every part of the body including the brain, liver and even on our immune cells! When estrogen interacts with these receptors, it can influence the behaviour of various immune cells (such as T cells, B cells, and macrophages) and regulate the release of inflammatory molecules, therefore impacting the immune system.
Estrogen can impact the immune system in the following ways:
- Estrogen and estrogen receptors can impact inflammatory mediators in allergic reactions (and estrogen itself actually increases histamine which can worsen allergic relationship, rashes, and perimenopause symptoms!)
- Estrogen and estrogen receptors also regulate the function of innate immune cells (our innate immunity).
- Estrogen has anti-inflammatory effects, where it can dampen inflammatory responses, this is seen in pregnancy for example.
- Estrogen has also been linked to inhibiting viral replication, although different viral infections seem to respond differently to estrogen and more research is needed here.
- Estrogen can influence the development and number of immune cells, including T regulatory cells, which are important for downregulating immune responses.
| We commonly see clients in menopause with increasing infections and viruses and unable to fight them off the way they previously could. One of the contributing factors to this is low estrogen levels impacting their immune system and inflammation regulation. |
Autoimmunity and estrogen
There is another side of estrogen and immunity that needs to be discussed. Although estrogen generally strengthens and bolsters the immune system’s response to pathogens, it can also stimulate the immune cells to produce more antibodies and in fact increase inflammatory response. In fact some sources state that women make up 80% of patients with autoimmune disorders, and hormones seem to be central to that.
High estrogen levels have been linked to autoimmune disease and allergic reactions (hello histamine and estrogen connection!). This is a complex matter as not only does it depend on estrogen levels, but also specific estrogen receptor activity, but also the specific type of immune cell that is involved, its activation state, and the local microenvironment all influence how estrogen affects the immune system.
Some autoimmune diseases like systemic lupus erythematosus (SLE), rheumatoid arthritis (RA) and multiple sclerosis are strongly linked in research to estrogen. Some conditions like SLE seem to be exacerbated with high estrogen, while interestingly RA seems to improve with higher estrogen for example in pregnancy which therefore reveals how estrogen impacts the immune system differently.
Progesterone and immunity
One of the most forgotten hormones that support your immune system is progesterone. Most people don’t realise the vital importance of progesterone past reproduction. Progesterone is vital for your mental health, bone health, sleep, brain, and your immune system. In fact progesterone is often nicknamed as an immune modulator as it essentially can help prevent the immune system from overreacting.

As we know progesterone is a key player in pregnancy, and one of its main jobs is to regulate the immune system during pregnancy, for example when the immune system must accept the embryo (essentially a foreign entity to the mother’s immune system because it contains paternal genes) but must do so without launching an attack against this foreign entity. Progesterone helps the body to navigate this by modulating the immune system.
So how does progesterone support or impact the immune system?
- Progesterone impacts the activity of immune cells such as T cells, natural killer cells and macrophages.
- Progesterone can impact immune cells and help create a more anti-inflammatory state
- Progesterone can act as an immunosuppressant (as explored above to accept the embryo)
- Progesterone influences the balance of inflammatory and anti-inflammatory cytokines, promoting a more immunotolerant state.
- Progesterone inhibits mast cell degranulation (which can counter high histamine issues with high estrogen – another reason it is vital to support ovulation and progesterone!).
What about when progesterone levels are high or low?
Like all hormones, there is always an optimal level to ensure a healthy activation of the immune system. When progesterone is too high we see some benefits such as the suppression of increased or heightened immune activity (autoimmune disease for example), which is why many women report a reduction in symptoms of their autoimmune disease in pregnancy. But on the other side of the coin, high progesterone is also linked to a suppression of anti-viral immune responses which can in turn increase the person’s susceptibility to certain infections.
Interestingly there is research that shows that in the luteal phase when progesterone levels are highest and in high progesterone states like pregnancy, the immunosuppressant actions of progesterone may in fact weaken the bodies response to certain infections, leaving a more more susceptible to viral infections for example.
If progesterone levels are lower this is associated with a more dysregulated immune system and an increased susceptibility to certain infections and even flares in autoimmune diseases. We see this in perimenopause when clients start to become low in progesterone and find they start picking up bugs and falling sick much more easily than they did before. Just another example of why testing your progesterone levels over 35 is so vital!
The luteal phase and period flu:
You may have heard of period flu or experienced it yourself, it’s when you feel nauseas, low-grade fever, headaches and joint pain right before your period – not so nice right? And actually has a lot to do with how your hormones interact with your immune system. Basically it is a combination of hormonal shifts, immune system changes and inflammatory responses before menstruation. Both estrogen and progesterone are low and therefore not providing you with the immune and anti-inflammatory benefits they normally do. Therefore this is another good reason to rest and take it easy in the luteal phase, and focus on extra sleep to keep the immune system happy too.
So does this mean immunity changes across the cycle?
Essentially yes, but of course as always there needs to be more research. As we have learnt the immune system is greatly impacted by hormones, like estrogen (high in the follicular phase) and progesterone (high in the luteal phase) but as these hormones fluctuate throughout the cycle of course the immune system will fluctuate too.
To summarise:
- In the follicular phase (estrogen reaches its peak) we see a more active and proinflammatory immune system activity
- As we move into the luteal phase as progesterone increases we see the immune system creating a more tolerant environment based on the immune modulating action of progesterone.
- In other words it might be summarised that the immune system focuses on immune tolerance rather than deference in the luteal phase.
| But quickly let’s not forget about our other hormones like testosterone, insulin and the thyroid hormones…. Testosterone: Testosterone, which although is considered the primary male hormone, is also vital for female health, has a more suppressive effect on the immune system. Essentially higher levels of testosterone levels can reduce inflammation but they may also dampen the body’s ability to respond quickly to pathogens. Thyroid Hormones: Thyroid hormones regulate metabolism, but they also influence immune cell activity. Both underactive (hypothyroidism) and overactive (hyperthyroidism) thyroid function can disrupt immune balance, affecting the body’s ability to fight infections and regulate inflammation. Insulin: Insulin, the hormone that regulates blood sugar, also impacts immunity. Poor insulin regulation, such as in insulin resistance, can lead to chronic low-grade inflammation. This inflammation impairs immune function, making infections more likely and slowing recovery. |
So where to from here?
So we have learnt that our hormones play a very complex and very important role in regulating our immune system. This is just one of the many reasons why we advocate so strongly for healthy, natural cycles and regular ovulation at FUTURE WOMAN.
| So here are your takeaways from this article: Hormones shape immune behaviour: Hormones like cortisol, estrogen, progesterone, actively influence how your immune system responds to threats. Progesterone rebalances but does not necessarily weaken immunity: During the luteal phase, progesterone promotes an anti-inflammatory, tolerant state that supports tissue repair and reproductive health. The menstrual cycle affects immune rhythms: Immune cell activity shifts across the cycle, with estrogen boosting certain defenses and progesterone calming inflammation. Hormonal imbalance can disrupt immunity: Ongoing stress, blood sugar swings, and poor sleep can throw hormones off hormone balance, making immune responses less efficient. Immune resilience depends on hormonal harmony: A well-regulated endocrine system supports steady, effective immune protection all month long. |
So what can you do?
The best thing you can do is TEST your hormones and address any imbalances with targeted support from an experienced practitioner. This way we can optimise YOUR hormone levels and support your immune system to support you all year long.