“Just take estrogen” has to be the most problematic perimenopausal advice I have come across. But, worryingly, it’s also the most common advice women receive from their doctors when they raise the topic of HRT in their 30’s and 40’s. This piece of advice has seen hundreds of women come to us at FUTURE WOMAN desperate to find some answers as to why they feel even worse even after trying HRT.
So why is this happening? Isn’t HRT supposed to help in perimenopause? Let’s take a look at the most common reason I see.
1) Perimenopause is being confused with menopause
The first mistake that is being made here is that providers and doctors are missing one key important fact: perimenopause is not menopause. This may sound obvious, but this mis-understanding or over simplification is causing the wrong prescription of HRT for many women. I see too many women in perimenopause being treated for menopause due to lack of proper testing and the tendency to treat everyone in this phase of life the same way.
What’s the difference between perimenopause and menopause?
Perimenopause is the 2-12 years BEFORE menopause and it is a time of fluctuating hormones.
We see perimenopause happening in four key stages, and each stage brings its own unique hormone picture.
First we see progesterone drop and decrease, causing most of the early perimenopause symptoms such as anxiety, poor sleep, brain fog and mood changes. Next we see estrogen changing, typically first INCREASING then fluctuating up and down across perimenopause. Finally, as we near the end of perimenopause estrogen does decrease and of course in menopause we see a low level of both estrogen and progesterone.
Read more about the 4 stages of perimenopause here.

So perimenopause is not a state of estrogen deficiency
So perimenopause is not actually a state of “estrogen deficiency” like menopause. As you can see from the chart below, especially in the early stages, estrogen can be higher than it has ever been, before eventually lowering close to menopause.
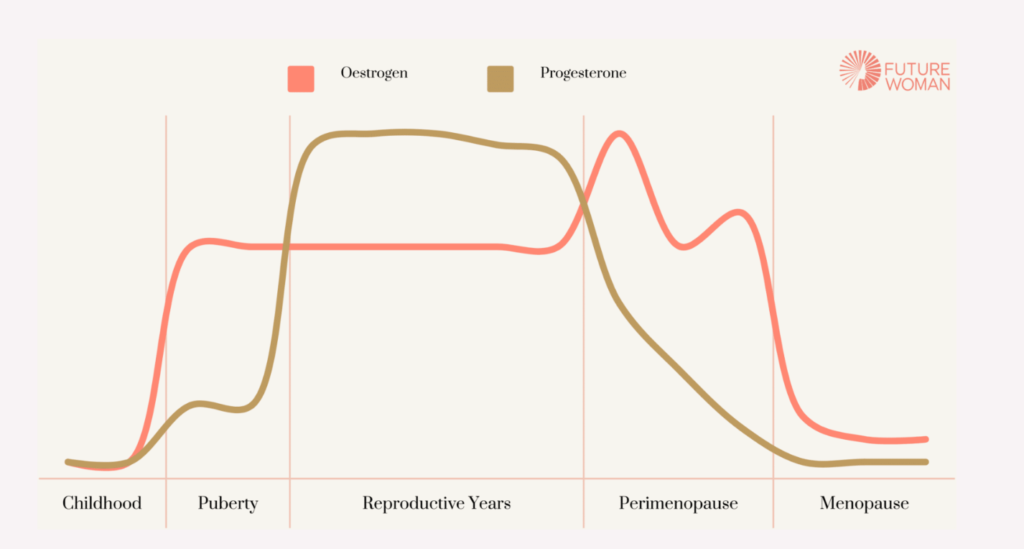
You may be able to see the common mistake easily now: giving estrogen to someone in perimenopause (especially early perimenopause) could be adding fuel to the fire and making things much much worse by sending estrogen too high while not addressing progesterone. Think increased headaches, migraines, mood swings, irritability, hot flushes, anger, new allergies and much more.
Women actually need an approach to HRT that evolves alongside their stage of perimenopause – assuming the same dose or combination of HRT will support you through all these fluctuations is fundamentally flawed.
2) There’s a medical bias towards estrogen
Estrogen has long been treated as the leading hormone, which is one reason estrogen HRT is prescribed more often. Even though research now highlights the crucial role of progesterone for both mental and physical health, thinking in medicine has been slow to shift. Estrogen still receives the most attention.
Part of this bias stems from history. Estrogen was discovered before progesterone, which immediately gave it scientific prominence. It was also easier to measure and its effects were straightforward to observe, such as the physical changes from puberty into the reproductive years.
Other factors contributed to estrogen’s dominance. Progesterone was harder to study because meaningful measurements depend on the timing of ovulation, while estrogen can be tracked across the whole cycle. Estrogen’s effects also appear more obvious at first glance, such as breast development, whereas progesterone often works in quieter ways that support bone health, sleep, immune regulation and the nervous system, even though symptoms like anxiety or heavy bleeding can be clear signs of imbalance.
Progesterone is still widely misunderstood and is often reduced to a pregnancy hormone. This has shaped treatment approaches. Body identical estrogen became the first line option for perimenopause and menopause, while progesterone is frequently substituted with a progestin that is used mainly to protect the uterus rather than to support the rest of the body.
3) Women aren’t given access to proper testing
Another reason that women typically receive a standardised HRT prescription for estrogen HRT is that they’re not given access to proper testing.
At best on the NHS you’ll receive two FSH tests in perimenopause 6 weeks apart. This is problematic for two reasons: firstly, it’s not useful for perimenopause. Like estrogen, your FSH levels will be fluctuating in perimenopause so getting a proper reading is only likely in the final stage of perimenopause and menopause. Secondly it doesn’t tell you anything about where estrogen and progesterone levels are before starting HRT – this needs rigorous testing, ideally in the luteal phase to determine the best approach for YOU. Your HRT will likely need to adapt as you progress through perimenopause.
Testing in perimenopause needs to be in depth and comprehensive to understand the individual’s picture. Read more here about testing in perimenopause.
4) No consideration is given to estrogen metabolism
Finally, one reason why estrogen HRT might leave you feeling worse in perimenopause is due to poor estrogen metabolism. If, in addition to high estrogen levels before starting HRT, you also have trouble metabolising your estrogen, then HRT will leave you feeling awful.
If you favour what we call the 4-OH or 16-OH pathways for estrogen detox you can be left with increased inflammation and oxidative stress in the body which can lead to symptoms like weight gain, sore breasts, anxiety, heavy periods and mood changes. Therefore it might not be your HRT levels, but the way you are detoxing your HRT.
Since this is a relatively new area of research, doctors will not consider estrogen metabolism before prescribing estrogen HRT.
Learn more about hormone metabolism.
Why this client felt awful on estrogen HRT
Sometimes it’s helpful to share an example, so I’ll share what happened to a recent client called Lydia.
She came to us when she was 42. She had been prescribed body identical estrogen and a synthetic progestin (not progesterone) by her GP after complaining of symptoms such as mood changes, irregular periods and very painful, heavy bleeding.
Since taking the HRT she was feeling more irritable, her breasts were tender, and her periods were even heavier. She also had hives for the first time in her life and noticed she was more sensitive to certain foods.
We tested with the Advanced Hormone Test and saw that Lydia had very high estrogen, poor estrogen metabolism and low progesterone. This left her with unopposed estrogen which was making her symptoms much worse.
She decided to add body-identical progesterone into her prescription (instead of the progestin) with the help of FUTURE WOMAN, and we recommended her some estrogen detox support. Within one cycle, she felt better. Eventually she even decided to come off the estrogen HRT completely and to monitor her estrogen through regular testing.
So what’s the best approach to HRT in perimenopause?
The first thing that needs to happen is wider education about what is actually happening in perimenopause and an understanding of the importance of progesterone in the early stages.
Secondly, each woman needs a personalised approach that involves comprehensive hormone and hormone metabolite testing before HRT prescription.
If women and health care providers deeply understand perimenopause, its four stages and the importance of hormone metabolism, this will result in proper prescription of HRT and meaningful improvement in symptoms.