Have you been feeling “off” lately but can’t quite pinpoint why? Perhaps you’re tossing and turning at night, dealing with unpredictable periods, feeling more anxious than usual or struggling with stubborn weight gain. Something you might not have considered is your low progesterone levels could be the missing piece of your health puzzle.
Low progesterone is surprisingly common. We estimate that at least 5 million women in the UK of reproductive age are deficient in this vital hormone, yet many women don’t realise this hormonal imbalance might be behind their most frustrating symptoms. Let’s explore what progesterone does, what counts as “low” and the tell-tale symptoms that suggest your levels might need attention.
What Is Progesterone, Really?
Before we dive into symptoms, let’s get clear on what progesterone actually does in your body. This hormone is so much more than just a “pregnancy hormone”. Think of progesterone as your body’s master regulator and protector, quietly orchestrating multiple essential functions.
Progesterone helps regulate your menstrual cycle, promotes restful sleep, stabilises your mood, protects your brain, supports bone health, modulates your immune system and influences how your body processes energy.
Progesterone is produced by your ovaries after ovulation, specifically by something called the corpus luteum, which forms where your egg was released. When progesterone falls short, multiple systems can suffer, producing a cascade of symptoms that can seriously impact your quality of life.
What Actually Counts as “Low” Progesterone?
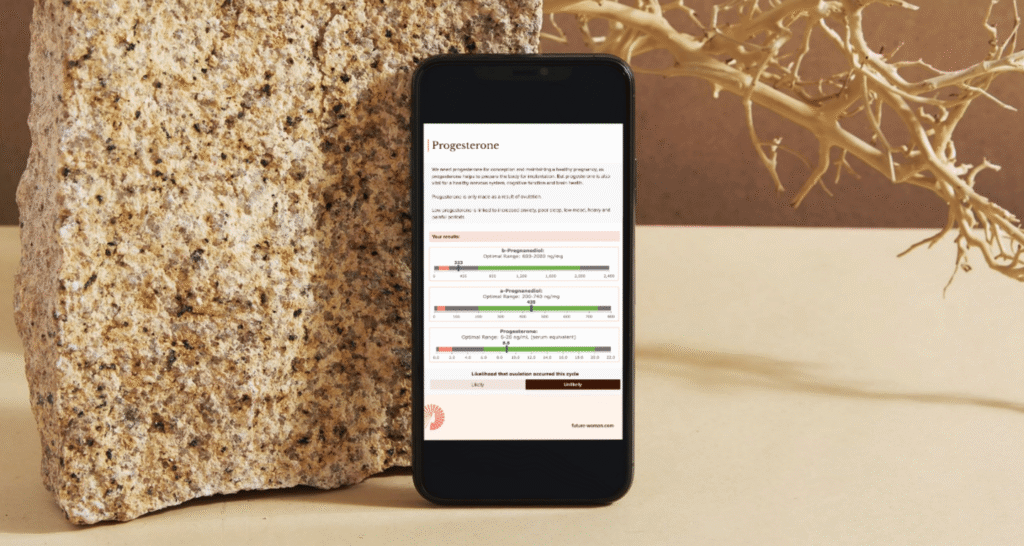
In clinical research, progesterone levels between 6 and 20 ng/mL are typically considered “normal” during your reproductive years and indicative of ovulation. However, at FUTURE WOMAN, we aim for levels of 10 ng/mL or higher in order to feel progesterone’s full body effects.
But it’s not just about the amount. How long you produce progesterone matters too. Your luteal phase (the time from ovulation to menstruation) should last 11–16 days. Anything shorter suggests your body isn’t producing progesterone for long enough to do its job properly.
Finally, progesterone must be assessed in relation to estrogen. In a healthy luteal phase, your body should ideally produce about 100 times more progesterone than oestrogen. When progesterone is low relative to oestrogen, it throws off downstream signalling in numerous systems throughout your body, making you more vulnerable to symptoms we’re about to explore.
Read more about estrogen dominance.
The Tell-Tale Signs: Common Symptoms of Low Progesterone
Irregular or Abnormal Menstrual Cycles
One of the most noticeable signs that progesterone might be low is changes to your menstrual cycle. Progesterone’s primary reproductive role is to maintain the second half of your cycle: the luteal phase. This is the period of time between ovulation and your period arriving. When levels are insufficient this phase may shorten to under 11 days, cycles can become unpredictable and you might experience spotting or breakthrough bleeding.
With poor or absent ovulation, which can occur with conditions like PCOS, chronic stress or thyroid dysfunction, your body fails to generate enough progesterone at all. Because progesterone supports the maturation and stability of your uterine lining (endometrium), a deficiency leads to early breakdown or shedding. Over time, this can contribute to hormonal imbalances, lower fertility and heavier compensation bleeding in subsequent cycles. If you’re tracking your cycles and noticing they’re consistently short or erratic, this is a red flag worth investigating.
Read more about common causes of irregular cycles.
Spotting or Breakthrough Bleeding
In conjunction with cycle irregularities you might notice spotting between periods, often pink or brown discharge that appears days before your period officially starts. This happens because insufficient progesterone means your endometrium lacks structural support. Think of progesterone as the scaffolding that holds your uterine lining stable; without adequate levels, the structure becomes unstable.
Even small drops in progesterone can destabilise the lining, causing light bleeding or spotting before your true period begins. This symptom is often dismissed as “normal,” but in context with other signs, it strongly suggests low progesterone.
Sleep Disruptions & Insomnia
If you’re lying awake at 3 AM wondering why sleep has become so elusive, low progesterone could be sabotaging your rest. Progesterone is metabolised into allopregnanolone, which enhances signalling of the calming, inhibitory GABAergic pathway in your brain that helps you wind down and drift off.
When progesterone falls, that sedative buffer weakens, making it harder to fall asleep or maintain deep, restorative sleep.
Women frequently report light, fragmented sleep, frequent awakenings, and waking feeling completely unrefreshed. Over time, these sleep deficits can disturb your hypothalamic-pituitary axis (the hormonal control centre in your brain), which further impairs progesterone production. It becomes a vicious feedback loop that heightens your sensitivity to stress, inflammation and circadian disruption.
Mood Swings, Anxiety & Depression
Do you feel you’re on an emotional rollercoaster in the week or two before your period? There’s solid science behind this. As we saw above, progesterone acts as a natural mood stabiliser through its metabolite allopregnanolone. When progesterone is low, estrogen often dominates, which may trigger irritability, anxiety or depressive symptoms.
Many women with PMS (premenstrual syndrome) or the more severe PMDD (premenstrual dysphoric disorder) struggle with mood instability and inadequate progesterone is frequently the underlying culprit. If you feel like you’re “not yourself” during certain parts of your cycle, or if small stresses feel overwhelming, your progesterone-estrogen balance deserves attention.
Read more about mood and hormones.
Persistent Fatigue & Low Energy
The fatigue tied to low progesterone is different from everyday tiredness, it’s a deeper, bone-weary exhaustion that doesn’t improve with rest. Progesterone supports thyroid regulation and the conversion of T4 to T3 (the more active form of thyroid hormone) in your tissues. When progesterone is insufficient, your metabolic rate may slow down, like turning down the dial on your body’s energy production.
Coupled with poor sleep and hormonal shifts, low progesterone often results in daytime exhaustion and impaired recovery. This fatigue frequently worsens across the day and may leave you feeling unable to exercise, socialise, or function at your best. Over time, limited energy can influence your exercise capacity, muscle tone, and downstream hormonal resilience.
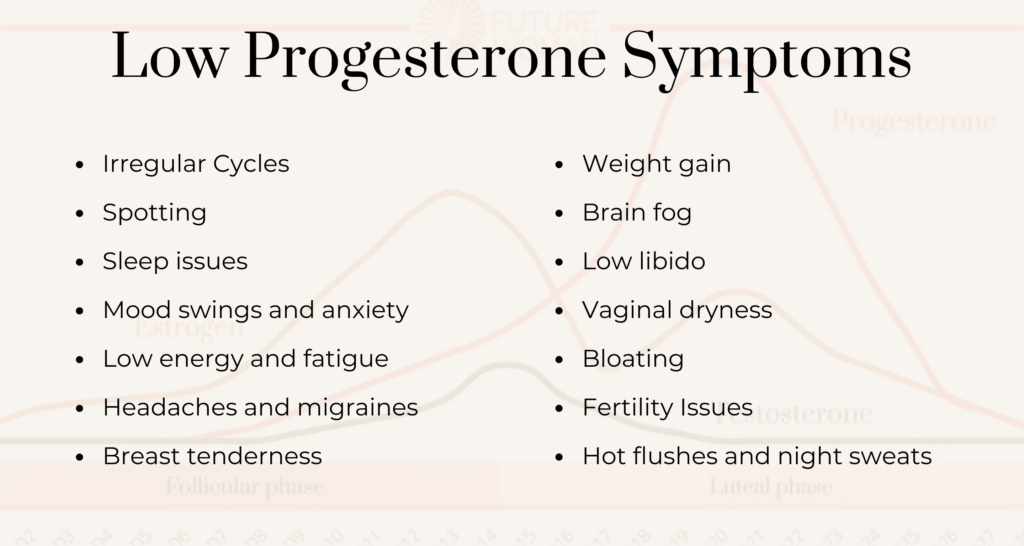
Headaches & Migraines
If you notice headaches or migraines that seem to follow your menstrual cycle, particularly in the days before your period, hormonal fluctuations are likely to blame. Precipitous drops in progesterone are well-known triggers for headaches and menstrual migraines.
Progesterone has vascular and neuroprotective actions that help regulate cerebral blood flow, dampen inflammation, and stabilise blood-brain barrier integrity. When levels plunge (especially in the late luteal phase or around menstruation), that protection weakens and migraines often follow. Many women notice reduced headache frequency once hormonal balance is restored. Interestingly, progesterone is even under investigation for its neuroprotective benefits in traumatic brain injury and vascular injury models-that’s how powerful its protective effects are.
Breast Tenderness & Fibrocystic Changes
Are your breasts feeling swollen, tender or lumpy, especially before your period? This often signals that estrogen is dominating relative to progesterone. Progesterone counteracts estrogen’s proliferative influence in breast tissue by moderating receptor expression and limiting excessive cell division.
When progesterone is low, estrogen can become relatively higher, stimulating fluid retention, tissue proliferation and cyst formation. This leads to swelling, pain and that lumpy texture many women find concerning. Clinical observations reveal that improving the hormonal balance of progesterone relative to estrogen significantly alleviates breast discomfort and may reduce the risk of fibrocystic changes over time.
Weight Gain, Especially Around the Middle
Struggling with stubborn weight gain, particularly around your midsection? Low progesterone shifts your metabolic balance towards storing rather than burning fuel. As progesterone declines, insulin sensitivity often weakens and cortisol or estrogen dominance may exacerbate visceral fat storage (that’s the belly fat that’s particularly unhealthy).
Studies in menopause literature show that hormonal transitions can lead to increased body fat and reduced energy expenditure. Moreover, some mechanistic research suggests that progesterone influences hepatic glucose output (sugar release from the liver), which may worsen blood sugar control in insulin-resistant states, making metabolic management even more challenging. If unexplained weight changes are frustrating you despite maintaining healthy habits, hormonal imbalance could be the hidden factor.
Read more about weight gain and hormones.
Brain Fog, Memory Decline & Poor Focus
Can’t remember where you put your keys, again? Feeling like your thinking is fuzzy or you can’t concentrate like you used to? Progesterone supports neuroplasticity (your brain’s ability to adapt and form new connections), synaptic resilience and protective signalling throughout your brain. When levels drop, those cognitive supports begin to weaken.
This manifests as memory lapses, difficulty concentrating, slowed mental processing, or general brain fog. In both animal and human studies, progesterone has been shown to protect neurons, promote synaptic and dendritic growth (the branching connections between brain cells), and dampen oxidative and excitotoxic stress processes, all critical for maintaining cognitive clarity. Loss of these protective pathways can accelerate mental “fogginess,” especially under hormonal or inflammatory stress.
Low Libido
Though testosterone often gets all the credit for sexual drive, progesterone plays a complementary role in hormonal balance, vascular tone and receptor crosstalk (how different hormones communicate in your body). When progesterone is insufficient, the hormonal environment may shift towards estrogen dominance or relative androgen deficiency, disrupting libido.
Add in the fatigue, mood instability, sleep loss and potential vaginal dryness that often accompany low progesterone and diminished sexual desire becomes a predictable downstream symptom. It’s rarely just one thing, it’s the cumulative effect of feeling off in multiple ways.
Vaginal Dryness & Discomfort
Whilst vaginal moisture is primarily driven by estrogen, progesterone also contributes to mucosal integrity, lubrication,and blood vessel support. A drop-in progesterone may reduce vaginal blood flow and weaken mucosal tissues, increasing friction, dryness, irritation or discomfort during sex, even when estrogen levels aren’t extremely low.
Over time, persistent dryness may impair mucosal health, increase infection risk and diminish sexual enjoyment. If you’re experiencing this symptom alongside others on this list, it’s worth considering the bigger hormonal picture rather than treating it in isolation.
Bloating & Fluid Retention
Ever feel like you’re “holding water” for no apparent reason? Progesterone helps regulate sodium and water balance through mild natriuretic effects (promoting salt excretion) and modulation of the renin-angiotensin-aldosterone system, the body’s complex fluid-balance mechanism.
When progesterone declines, its moderating influence wanes and your body retains more sodium and fluid. This often appears as bloating, puffiness, swelling of the abdomen, limbs, or face and it can fluctuate with your cycle. Though often dismissed, this retention can aggravate discomfort, mask weight changes on the scales and worsen cramps or digestive sluggishness.
Fertility Issues & Early Pregnancy Loss
If you’re trying to conceive or have experienced pregnancy loss, this section is particularly important. Progesterone is absolutely essential after ovulation. It transforms the endometrium into a receptive, secretory state, supports implantation and sustains early pregnancy until the placenta takes over hormone production.
When progesterone is too low, the uterine lining may not mature sufficiently, implantation may fail, or early miscarriage may occur. Persistent luteal deficiency (inadequate progesterone production during the luteal phase) is considered a key factor in recurrent pregnancy loss. If you’ve experienced multiple early losses, testing your progesterone levels and luteal phase length should be a priority.
Hot Flushes & Night Sweats
Although low oestrogen is the classic driver of hot flushes, low progesterone can exacerbate your body’s ability to maintain a stable temperature. Progesterone has vasoregulatory and thermogenic properties that help stabilise your core temperature.
When levels dip, your body’s internal “thermostat” can misfire, provoking sudden heat, flushing and night sweats, especially during sleep. These symptoms frequently worsen hormonal and sleep disturbances, compounding fatigue, mood instability and daily disruption. If you’re experiencing these symptoms but haven’t yet reached menopause, progesterone deficiency might be the culprit.
What Causes Low Progesterone?
Understanding the symptoms is crucial, but you might be wondering why your progesterone is low in the first place. Low progesterone rarely happens in isolation, it’s usually the result of one or more underlying factors. Here are the most common causes we see at FUTURE WOMAN:
- Ovulation Issues: Conditions like Hypothalamic Amenorrhea (HA) or Polycystic Ovarian Syndrome (PCOS) mean your body isn’t ovulating and therefore not forming a corpus luteum, so progesterone production is compromised or absent.
- Perimenopause/Menopause: As you approach menopause, ovulation becomes less predictable and progesterone production naturally declines, often before estrogen levels drop significantly. Learn more about the four stages of perimenopause.
- Hormonal Contraceptive use: These synthetic hormones actually suppress your own natural hormones to prevent ovulation and pregnancy. The synthetic progestins, also in the hormonal coil, implant and injection, do not offer the same wide reaching benefits as natural progesterone and can actually have negative effects on the body.
- Chronic Stress & Elevated Cortisol: This is a big one. High cortisol levels from chronic stress can interfere with progesterone production. An overactive HPA axis due to chronic stress can suppress the hypothalamic-pituitary-gonadal (HPG) axis, the system that regulates sex hormone production. This can result in lower levels of sex hormones like estrogen, progesterone, and testosterone.
- Obesity: Excess body fat, particularly visceral fat, can disrupt hormonal balance and interfere with normal ovulation and progesterone production.
- Under-Eating or Over-Exercising: Both extremes signal to your body that resources are scarce, which can suppress ovulation as a protective mechanism. No ovulation means no progesterone.
- Poor Nutrition: Inadequate intake of key nutrients needed for hormone production, including B vitamins, magnesium, zinc, and healthy fats, can compromise progesterone synthesis.
- Hypothyroidism (Underactive Thyroid): Your thyroid and reproductive hormones are intimately connected. When your thyroid is sluggish, it can interfere with ovulation and progesterone production. Read more about symptoms of thyroid imbalances.
- Hyperprolactinaemia (Elevated Prolactin): High prolactin levels, which can be caused by stress, certain medications or pituitary issues, can suppress ovulation and therefore progesterone production.
- Low Cholesterol: This might surprise you, but cholesterol is the building block for all your steroid hormones, including progesterone. Excessively low cholesterol can limit hormone production.
The Bottom Line for Low Progesterone
Key Takeaway
Low progesterone is far more common than most people realise, and it can profoundly impact your quality of life in ways that extend throughout your entire body. From sleep and mood to metabolism, brain function and menstrual regularity, progesterone is truly a whole-body hormone that deserves attention.
If you’ve been struggling with any of these symptoms, don’t dismiss them as something you have to live with. Getting your progesterone levels checked with the Advanced Hormone Test (at the right time in your cycle, in relation to estrogen) could be the key to finally feeling like yourself again. Our testing comes with a 12 week transformational nutrition plan to improve your symptoms.
With proper testing, investigation and targeted support, most women experience significant improvement in their symptoms and overall quality of life.
References
Backstrom, T., Bixo, M., Johansson, M., Nyberg, S., Ossewaarde, L., Ragagnin, K., Savic, I. (2003). The role of hormones and hormonal treatments in premenstrual syndrome. CNS Drugs, 17(5), 325–342. https://pubmed.ncbi.nlm.nih.gov/12665391/
Baker, F. C., Lampio, L., & Driver, H. S. (2021). Sleep and menstrual-related disorders. Sleep Medicine Reviews, 57, 101434.
Brinton, R. D., Thompson, R. F., Foy, M. R., Baudry, M., Wang, J., Finch, C. E., et al. (2008). Progesterone receptors: form and function in brain. Frontiers in Neuroendocrinology, 29(2), 313–339.
Caufriez, A., Touitou, Y., de la Myser, J., & Meunier, J. (2011). Progesterone prevents sleep disturbances and modulates GH, TSH, and melatonin secretion. Journal of Clinical Endocrinology & Metabolism, 96(4), E614–E623.
Davis, S. R., Davison, S. L., Donath, S. M., & Bell, R. J. (2008). Circulating androgen levels and self-reported sexual function in women. JAMA, 294(1), 91-96.
Freedman, R. R. (2014). Menopausal hot flashes: mechanisms, endocrinology, treatment. Journal of Steroid Biochemistry and Molecular Biology, 142, 115–120.
Hantsoo, L., Grigoriadis, S., & Epperson, C. N. (2017). Progesterone metabolites and mood symptoms. Current Psychiatry Reports, 19(12), 94.
Kingsberg, S. A., Wierman, M., Sarrel, P., et al. (2015). Female sexual dysfunction—medical and psychological treatments. Journal of Sexual Medicine, 12(12), 2465–2478.
Kumar, S., Mehta, A., & Das, S. (2010). Biological underpinnings of breast cancer. British Medical Bulletin, 94(1), 113–134.
Lancel, M., Faes, P., & Lazdunski, M. (1996). Progesterone induces changes in sleep comparable to those of agonistic modulators of the GABAA_AA receptor. American Journal of Physiology, 271(4), E763–E772.
MacGregor, E. A. (2015). Migraine management during menstruation and menopause. Continuum, 21(4), 990–1003.
Martin, V. T., Behbehani, M. M., & Bergmark, B. A. (2014). Mechanisms in endocrinology: sex hormones and headaches. European Journal of Endocrinology, 171(6), R223–R230.
Miracare. (n.d.). Importance of the progesterone (luteal) phase. Retrieved from Miracare fertility resources.
My Cleveland Clinic. (2023, January 16). Low Progesterone: Causes, Symptoms, Tests & Treatment. Retrieved from https://my.clevelandclinic.org/health/diseases/24613-low-progesterone
Plu-Bureau, G., Desreux, J., Lares, A., & Pallardy, G. (2006). Hormonal therapy and breast fibrocystic disease. Gynecological Endocrinology, 22(11), 635–638.
Prior, J. C. (2005). Ovarian aging and the perimenopausal transition. Journal of Obstetrics and Gynaecology Canada, 27(7), 682–695.
Rapkin, A. J., Mikose, R., & Case, A. F. (2012). The role of allopregnanolone in premenstrual dysphoric disorder. CNS Spectrums, 17(1), 39–47.
Sherwin, B. B. (2012). Estrogen and cognitive functioning in women: lessons we have learned. Behavioral Neuroscience, 126(1), 123–127.
Sovijit, W. N., Sovijit, W. E., Pu, S., Usuda, K., Inoue, R., Watanabe, G., Yamaguchi, H., & Nagaoka, K. (2021). Ovarian progesterone suppresses depression and anxiety-like behaviors by increasing the Lactobacillus population of gut microbiota in ovariectomized mice. Neuroscience Research, 168, 76–82.
Soules, M. R., Sherman, S., Parrott, E., et al. (2001). Executive summary: Stages of Reproductive Aging Workshop (STRAW). Fertility and Sterility, 76(5), 874–878.
Stachenfeld, N. S. (2008). Progesterone modulation of fluid balance. American Journal of Physiology – Regulatory, Integrative and Comparative Physiology, 294(3), R691–R696.
Thurston, R. C., Sutton-Tyrrell, K., Everson, R. B., et al. (2008). Endothelial function and white matter hyperintensities in midlife women. Stroke, 47(11), 2810–2815.
Verdier-Sévrain, S., Bonte, F., & Gilchrest, B. (2006). Biology of estrogens in skin: implications for skin aging. Experimental Dermatology, 15(2), 83–94.