Fibroids affect millions of women worldwide. They are often accompanied by difficult side effects like bloating, pain and heavy bleeding.
In this article we will find out exactly what fibroids are, the typical signs and symptoms, as well as the underlying hormonal drivers. Finally, we’ll look at how to treat fibroids and some easy tips you can start straight away at home.
Quickly find what you need
What are fibroids?
Uterine fibroids (also called leiomyomas) are benign solid tumours that emerge from a single uterine smooth muscle cell. It is important to note, there is no link between fibroids and uterine cancer.
Fibroids can grow anywhere in the womb and vary in size considerably – from the size of a grain of rice, to the size of a melon.
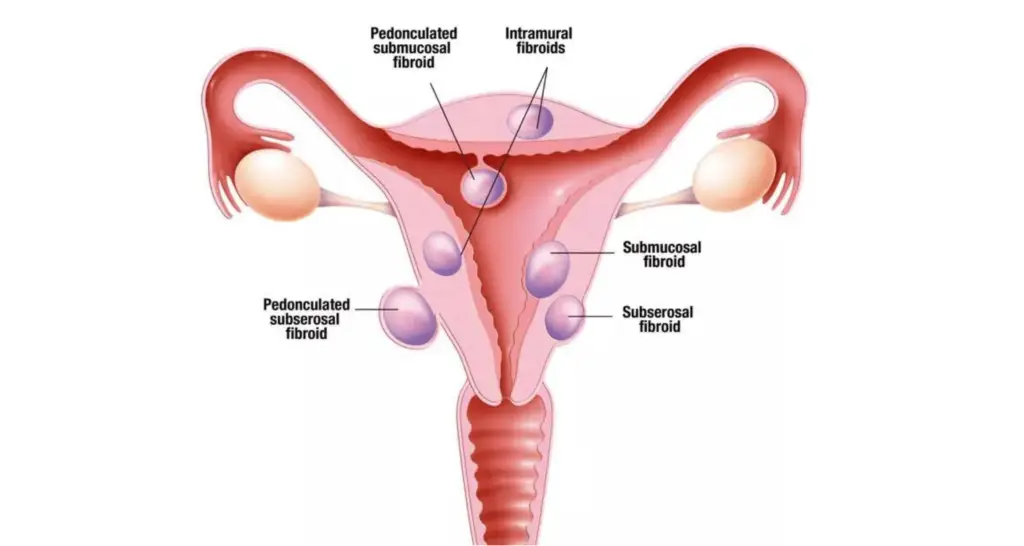
Types of fibroids include:
- Fibroids that develop in the muscle wall of the womb (intramural fibroids). These are the most common type of fibroid.
- Fibroids that develop outside the wall of the womb into the pelvis and can become very large (subserosal fibroids).
- Fibroids that develop in the muscle layer beneath the womb’s inner lining and grow into the cavity of the womb (submucosal fibroids).
- Sometimes subserosal or submucosal fibroids can be attached to the womb with a narrow stalk of tissue (pedunculated fibroids).
How common are fibroids?
Fibroids are extremely common and are found in 70–80% of women at some point in their lives. They most often present during years pre-or peri-menopause, around 30 to 50 years old.
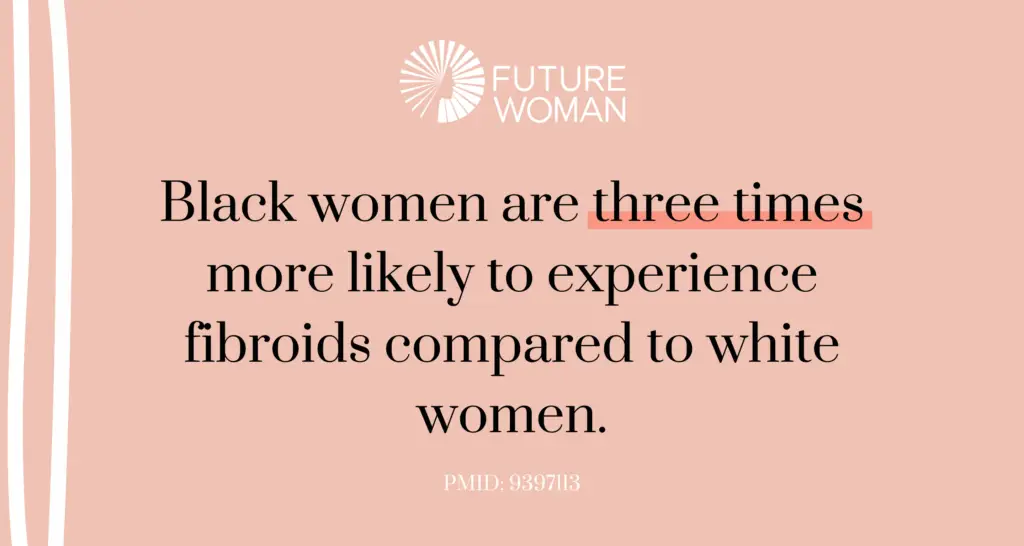
Fibroids are more prevalent in Black women and they typically present earlier, are more numerous, and are often larger in size. Whilst fibroids among White women typically arise later in life, with fewer and smaller fibroids.
It has been shown that there is a significant relationship between the presence of uterine fibroids and coexisting gynecological diseases. So, if you have endometrial polyps, endometriosis, PCOS and ovarian cysts amongst others, you could be at more risk of developing fibroids.
What are the symptoms of fibroids?
Approximately 30% of women with fibroids will present with severe symptoms that impact their daily lives. These can include:
- Abnormal menstrual bleeding (usually heavy periods)
- Anaemia (from heavy periods)
- Pain during periods
- Chronic vaginal discharge
- Bloating
- Pelvic pain and pressure
- Pain during intercourse
- Back pain
- Fatigue
- Urinary frequency changes
- Constipation
- Fertility issues
Symptoms can be dependent on the size, location and number of fibroids that a woman has.
If your doctor thinks you may have fibroids, they’ll usually refer you for an ultrasound scan to confirm the diagnosis.
Causes and drivers of fibroids
The exact cause of fibroids is unknown, but it is believed to be a combination of genetic, hormonal, and environmental factors.
There are several risk factors known to play a role in the development of fibroids including early onset of menstruation, late onset of menopause, vitamin D deficiency, obesity, no previous pregnancies and high blood pressure.
The following factors may drive the development, growth and symptoms of fibroids:
1) High estrogen
One of the biggest drivers for fibroid development and growth is high estrogen levels or poor estrogen detoxification. Research suggests each fibroid develops from an abnormal muscle cell in the uterus and multiplies rapidly when encountering estrogen, which promotes its growth. Fibroids have also been shown to have more estrogen receptors than the surrounding tissue.
Find out more about high estrogen and estrogen dominance here.
There are many ways estrogen has been shown be involved in driving fibroids;
- Age: Fibroids are not seen before puberty or after menopause, demonstrating estrogens’ role in their development.
- Aromatase expression: Aromatase is an enzyme that converts androgens into estrogens. It is thought that some women can over express this enzyme, causing higher levels of estrogen. There is evidence that aromatase is over expressed in fibroid tissue.
- Obesity: The ovaries produce the majority of estrogens in women before menopause, however estrogen can also be made and secreted by white adipose tissue (fat tissue). So, having a high amount of body fat can lead to high estrogen levels.
- Endocrine disrupting toxins: Synthetic xenoestrogens are endocrine disrupting chemicals which act like estrogen in the body, leading to higher levels of estrogen. BPA and phthalates are examples of xenoestrogens found in plastic but others can be found in cleaning products, pesticides and hygiene products such as shampoos. Research has actually found fibroid risk was stronger among more frequent users of personal care products. Find out more about Environmental Toxins and hormone health here
Testing your estrogen levels and estrogen detoxification with a comprehensive hormone test like the Advanced Hormone Test can help you understand if high estrogen is a factor for you.
2) Poor estrogen detoxification
Overall estrogen levels only provide part of the picture. It’s important also to look at overall estrogen detoxification (sometimes called estrogen metabolism).
In the first phase of estrogen detoxification, our estrogen can travel down three different pathways: the 2-OH, the 4-OH and the 16-OH.
The 16-OH-E1 binds more tightly to estrogen receptors than the other metabolites. If too much estrogen is metabolised down this pathway, then it may lead to increased fibroid growth as well as other symptoms such as heavy bleeding and breast tenderness.
Estrogen detoxification can only be tested in a urine test like the Advanced Hormone Test, it can be detected in blood serum.
Find out more about estrogen metabolites and how they are metabolised here.

3) Stress and the HPA axis
Dysregulation of the hypothalamic-pituitary-adrenal (HPA) axis (which produces and regulates our stress hormone cortisol) can cause disturbances to our sex hormones. For example, high cortisol levels have been shown to delay ovulation, which in turn causes low progesterone and unopposed estrogen. This can drive the growth of fibroids or make the symptoms of them worse.
4) Progesterone
As we have seen, low progesterone levels can lead to the effects of estrogen being magnified (what we call unopposed estrogen) and make the symptoms of fibroids worse. Ideally, progesterone should be around 100x higher than estrogen in the second half of the cycle.
Find out more about low progesterone and estrogen balance here.

Recently, progesterone itself has been implicated in the development and growth of fibroids. Progesterone receptors have been shown to be overexpressed in fibroid tissue compared to surrounding tissue, especially in smaller fibroids.
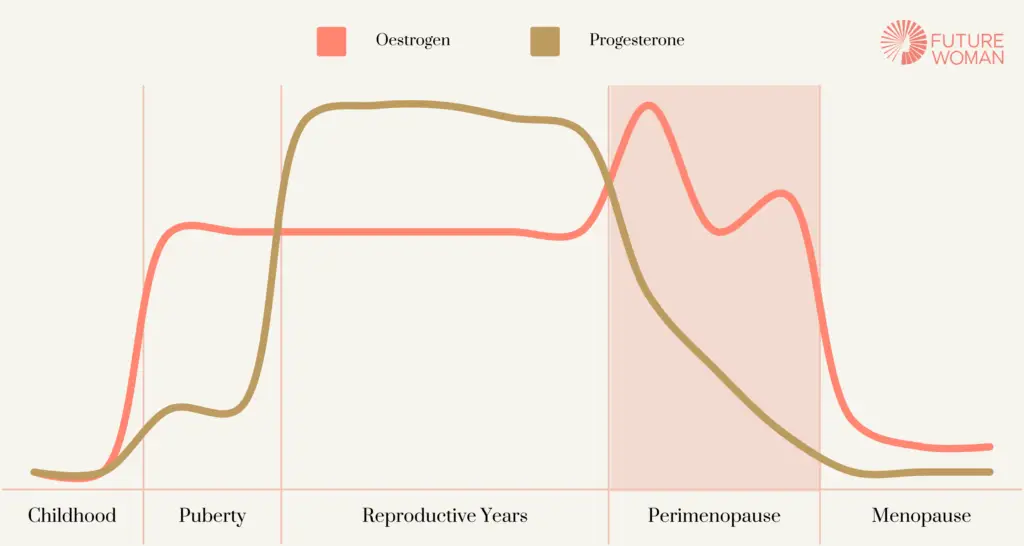
5) Perimenopause
Many people assume that when they start the transition into menopause (aka perimenopause), it is a decline in estrogen that is causing their symptoms.
However, in the early stages of perimenopause often progesterone is the first hormone level to drop, as ovulation becomes more sporadic. Estrogen can actually fluctuate wildly up and down, sometimes rising higher than at any other time in our reproductive lives. Therefore, estrogen dominance is extremely common in the early stages of perimenopause, and as we have seen, it is estrogen that drives fibroids.
You can read more about the signs and symptoms of perimenopause and the four stages of perimenopause.
Perimenopause, HRT and testing
For women with fibroids, the right HRT dose and regimen is crucial to avoid fibroid growth and the symptoms possibly related to it.
If you’re considering HRT in perimenopause, it’s important to test your hormones with a comprehensive hormone test first to understand which hormones you actually need. Many women are prescribed estrogen hormone therapy in perimenopause, balanced by a synthetic progestin. However, as we have seen, it’s likely you’re experiencing high estrogen and low progesterone in early perimenopause, so this combination will just compound estrogen dominance, making fibroids and their associated symptoms worse.
6) Early contraceptive use
Interestingly, oral contraceptive use at an early age (between 13-16 years old) has been shown to increase the risk of fibroids.
Treatment of fibroids
Treatment of fibroids in the NHS
Hormonal contraception
Contraceptive use, in general, has been shown to decrease the risk of getting fibroids as they suppress the hormones which have been shown to drive fibroids; estrogen, progesterone and testosterone.
However, while the contraceptive pill can help with the symptoms of fibroids, such as heavy bleeding, it does have its downsides. By suppressing your hormones, you are missing out on all the benefits that your natural hormones provide. Estrogen plays an important role in maintaining your cardiovascular, reproductive and bone health whilst progesterone reduces inflammation, has a calming effect on the body, helps with sleep and supports the thyroid, bones and brain. The oral contraceptive pill has also been shown to cause an imbalance in the gut microbiome, cause nutrient deficiencies and have a negative impact on bone density.
Other treatment options
Surgeries such as hysterectomy and myomectomy remain the first-line treatment for severe cases of fibroids, with few alternative long-term medical treatment options.
Treatments can also include painkillers, vitamin D3, hormonal contraceptives, gonadotropin-releasing hormone (GnRH) agonists, and drugs modulating the estrogen receptors.
Treatment of fibroids at FUTURE WOMAN
In order to address the underlying drivers of your fibroids, we would first recommend testing with a comprehensive hormone test such as the Advanced Hormone Test.
At FUTURE WOMAN, all our hormone tests are paired with a personalised healthplan prepared by expert nutritionists. This means that we can recommend specific supplement, diet and lifestyle advice to target the underlying drivers of your fibroids for lasting change.
Some markers which we would focus on include:
- Estrogen: As we have seen, estrogen can fuel the growth of fibroids, so we would look at your overall estrogen levels to see if they are elevated.
- Phase 1 estrogen metabolism: As we have seen, we’re specifically interested in the 16-OH pathway which is more likely to be elevated.
- Progesterone: As well as indicating whether or not ovulation took place, the balance of progesterone to estrogen is key. We are looking for progesterone to be at least 100x higher than estrogen in the luteal phase of the cycle (the second half).
- Androgen levels, including testosterone and androstenedione. As we have seen, they can be aromatised into estrogens. So elevated androgens can lead to elevated estrogens.
- Cortisol and the HPA axis: We look at free cortisol, your daily cortisol pattern and metabolised cortisol to get a clear picture of your HPA axis. An elevated cortisol pattern would usually indicate current stress whereas very low cortisol might indicate more of a long term stress picture.
- Quinolinate: This marker correlates with phthalate metabolite concentrations, which we have seen can be a risk factor for fibroids.

The Advanced Hormone Test
- Comprehensive and accurate hormone testing from home
- Expert interpretation
- Personalised supplement, diet and lifestyle recommendations
3 easy tips to help with fibroids
- Test and address your unique hormone imbalances. Understand if a hormone imbalance could be driving your fibroids and their symptoms and address those directly with a qualified practitioner like those at FUTURE WOMAN. Is it low progesterone? High estrogen? Sluggish estrogen metabolism? Or all 3?
- Remove ALL fragrances. This means candles, scented body wash, scented body creams, scented soaps, scented cleaning products and more. You can always add a few drops of essential oils to unscented products to make them smell amazing! You can find some great alternatives on our FUTURE WOMAN shop.
- Ditch or reduce alcohol. Alcohol can impact many areas of hormone health, but especially estrogen detoxification. Drinking any alcohol can disrupt and slow down this detoxification process leading to higher estrogen levels in the body.
References
Alsharif, S. A., Baradwan, S., Alshahrani, M. S., Khadawardi, K., AlSghan, R., Badghish, E., Bukhari, I. A., Alyousef, A., Khuraybah, A. M., Alomar, O., & Abu-Zaid, A. (2024). Effect of Oral Consumption of Vitamin D on Uterine Fibroids: A Systematic Review and Meta-Analysis of Randomized Clinical Trials. Nutrition and cancer, 76(3), 226–235.
Bariani, M. V., Rangaswamy, R., Siblini, H., Yang, Q., Al-Hendy, A., & Zota, A. R. (2020). The role of endocrine-disrupting chemicals in uterine fibroid pathogenesis. Current opinion in endocrinology, diabetes, and obesity, 27(6), 380–387.
Donnez J. (2020). Uterine Fibroids and Progestogen Treatment: Lack of Evidence of Its Efficacy: A Review. Journal of clinical medicine, 9(12), 3948.
Giuliani, E., As-Sanie, S., & Marsh, E. E. (2020). Epidemiology and management of uterine fibroids. International journal of gynaecology and obstetrics: the official organ of the International Federation of Gynaecology and Obstetrics, 149(1), 3–9.
Kwas, K., Nowakowska, A., Fornalczyk, A., Krzycka, M., Nowak, A., Wilczyński, J., & Szubert, M. (2021). Impact of Contraception on Uterine Fibroids. Medicina (Kaunas, Lithuania), 57(7), 717.
Moro, E., Degli Esposti, E., Borghese, G., Manzara, F., Zanello, M., Raimondo, D., Gava, G., Arena, A., Casadio, P., Meriggiola, M. C., & Seracchioli, R. (2019). The Impact of Hormonal Replacement Treatment in Postmenopausal Women with Uterine Fibroids: A State-of-the-Art Review of the Literature. Medicina (Kaunas, Lithuania), 55(9), 549.
Sun, K., Xie, Y., Zhao, N., & Li, Z. (2019). A case-control study of the relationship between visceral fat and development of uterine fibroids. Experimental and therapeutic medicine, 18(1), 404–410.
Volovsky, M., & Segars, J. (2021). A simplistic approach to fibroids is outdated. F&S reports, 3(1), 11–12.







